News
New Zealanders are not yet ready for widespread COVID-19 cases
29 Dec 21

New Zealanders are not yet ready for a widespread outbreak of COVID-19 cases.
New research finds:
- 37%, or around 1,479,000 adults are not confident they have the space needed to isolate at home if they get infected.
If the infection rate reaches the worst-case Government-modelled scenario of 16,000 infections a week, for the Delta strain only:
- 6,000 adults per week, or 300,000 a year may not live in places where the infected can have a bedroom to themselves and keep 1 metre away from others, creating a large demand for managed isolation.
In addition
- 6% of adults say they are not capable of caring for themselves at home if infected with COVID-19. If the 16% who are not sure if they are capable are included, it equates 3,500 a week of 16,000 infected or 183,000 adults per year.
The Horizon Research study, conducted in association with Auckland University’s School of Population Health between November 30 and December 6, 2021, indicates the country’s COVID-19 government and private primary health services could be overwhelmed by Delta cases alone.
The worst-case scenario of up to 16,000 infected per week with Delta is based on 90% of the total population aged 12 or more having had two doses of a COVID-19 vaccine. It models infection with the Delta strain, not the newly emerged Omicron strain which is far more infectious.
However, if the new strain Omicron spreads widely in the community, initial modelling projects as many as 20,000 to 60,000 people per day could be infected. The 20,000 per day projection is based on everyone who has had two doses of a COVID-19 vaccine having had a booster dose.
The Horizon survey also looked at how many New Zealanders knew what to do if they got a positive test result, if they had or would stock up on essential supplies to cover up to 14 days being isolated at home, and what health and other services they would need, including if their symptoms got worse.
Professor Chris Bullen, a Professor of Public Health at the University of Auckland’s School of Population Health, says the survey indicates the potential demand for the Government-and other services to support those self-isolating could be very high.
“The country needs to be prepared for high demand on healthcare and support services. Large numbers will be calling their own doctors, government healthcare support and ambulances if their symptoms worsen at home.
“If Omicron infections spread and that strain is less severe than Delta, though that is not yet certain, then clinical care might be easier – but the number needing care at home could be overwhelming,” Professor Bullen says. “Many have not stocked up on essential supplies, including medicines, to self-isolate for up to 14 days – and many actually say they will refuse to. Overall, 71% of adults need or want more information on the essential supplies they need to stock up on. Only 16% are fully prepared.”
The new study finds:
 Caring for self at home
Caring for self at home
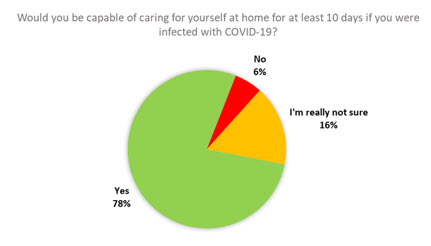
The majority of adults 18+ say they would be able to care for themselves at home for at least ten days if they were infected with COVID-19 (78%). 6% say they would not, and 16% are not really sure.
If there are 16,000 Delta infections per week, then this means up to 900 people every week would be unable to care for themselves at home, or 47,400 every year.
This indicates high likely demand for managed isolation.
If the 22% who are unsure are added to this, the figures are 3,500 per week and 183,900 per year.
- 6% = 226,000 adults 18+ who say they would not be able to care for themselves at home if they were infected.
- 22% = 650,300 who are not sure. Some of those – perhaps a majority – will also be unable to care for themselves either.
Space at home to isolate
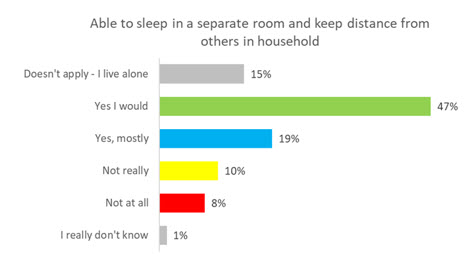
47% of people say they would be able to sleep in a separate room and keep at least 1 metre's distance from others in their household if they were isolating at home with a COVID-19 infection.
Another 19% say they would mostly be able to. 10% say that it would not really be possible, and 8% say it would not at all be possible.
This means that 37% of the adult 18+ population are not confident they have the space to safely isolate at home. This is equates to around 1,479,100 adults.
If there are 16,000 infections per week, this equates to 6,000 cases per week where the person infected is not sure they would be able to sleep in a separate room and keep at least 1 metre's distance from others in their household.
This could result in over 300,000 cases per year where people are unable to safely isolate at home. It projects large potential demand for isolation outside of the home.
What people want if they find they are infected
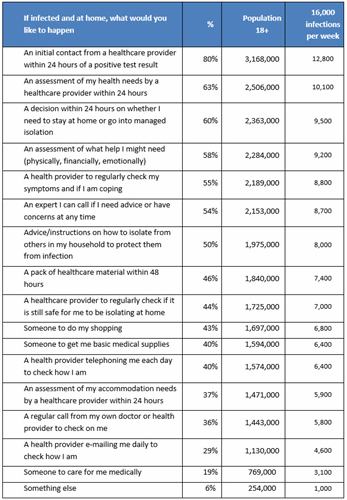
Most people selected multiple options of the things they would like to happen if they were infected with COVID-19 and isolating at home.
The mean number of items selected from a list of 17 is 7.6, which suggests people want many things to happen if they get infected.
This tables indicates how many adults prefer each type of support and the weekly demand for each activity or service if 16,000 pr week are infected.
On this basis 12,800 infected people per week will need individual contact from healthcare providers and 10,100 would expect an assessment of health needs within 24 hours.
9,500 a week will prefer a decision within 24 hours on ether they stay at home or go into managed isolation, and there will a large demand (9,200 adults per week) for an assessment of physical, financial and emotional needs). Almost half – 46% – want a healthcare pack within 48 hours.
Demand will extend from government healthcare services to general practitioners: of every 16,000 infected per week 5,800 want a regular call from their GP of health care provider to check on them.
If symptoms worsen
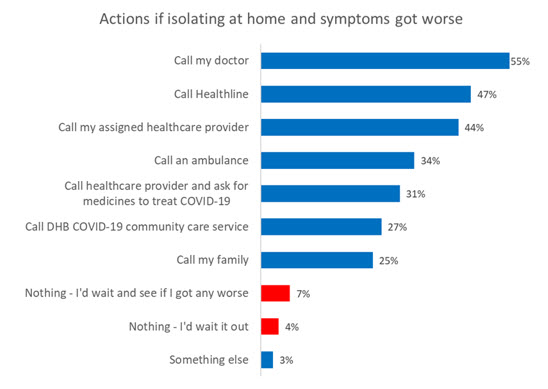 Most people would take several courses of action if they were isolating at home because of a COVID-19 infection and their symptoms got worse, with a mean of 2.6 actions selected from nine listed.
Most people would take several courses of action if they were isolating at home because of a COVID-19 infection and their symptoms got worse, with a mean of 2.6 actions selected from nine listed.
It is unknown at this stage the proportion of cases that might experience “worse symptoms” and so population projections cannot be calculated with any certainty.
However, the results again indicate high demand for health support and primary care support, including from outside the public health system.
55% would call their doctor, 47% call Healthline, 44% their assigned public healthcare provider, 34% would call an ambulance (potentially overloading local ambulance services) and call their family (25%).
New Zealanders are not prepared
Stocking up in case
Only 16% of people say they are fully prepared and stocked up on medicines and essential food and other supplies in case they need to self-isolate at home for 14 days. Another 35% say they are partly prepared.
However, 17% say they haven’t yet (but will), 21% say they didn’t know they might have to, and 11% said they have not and will not.
This means that 848,600 people [1] are unaware they might have to stock up, and 424,300 say they are not going to.
Essentials needed to self-isolate
The majority of people would like some more information about what is needed to self-isolate.
- 33% say they know, but would like more information = 1,296,700 adults 18+
- 33% don’t know – and would like more information = 1,300,600 [2]
- 5% don’t know – and say it shouldn’t be up to me = 214,100
This is a total of around 2,811,400 adults 18+ who need or want more information about what is needed for them to self-isolate at home. That is 71% of the adult population.
Knowledge of and belief in what might happen
Worst case Delta projections
Six of out 10 adults are not fully aware of worst-case COVID-19 modelling which projects up to 16,000 people could be infected with Delta per week.
40% say they are fully aware of the projections, or have some level of knowledge or heard of them (45%). 15% were not aware of these projections at all.
However, this means 60% are not fully aware, the equivalent of 2,363,305 people:
- 22% who didn’t realise they could get so high = 856,500 adults 18+
- 23% who had heard of it but not the detail = 900,100
- 15% who were unaware = 606,700.
Belief in worst case Delta scenario
One-third of people believe the government modelling for the worst-case Delta scenario could be correct (34%) and another third think there will be infections but not that high (35%).
23% disbelieve the modelling entirely, and another 8% are unsure.
This means that 66% of adults 18+ don’t believe the modelling – either at all, or not entirely, or just don’t know. This is 2,605,300 adults:
- 34% who think it could be correct = 1,360,100 adults 18+
- 35% who think it won’t get that high = 1,403,700
- 23% who don’t believe it at all = 892,200
- 8% who aren’t sure = 309,300
The lack of belief affects behaviour: 6% of those who believe it are saying they won’t stock up in case they have to isolate at home, compared to 17% of those who don’t believe it at all.
People who are unvaccinated and do not have an appointment booked are much more likely to disbelieve the modelling – 62%.
Public-interest research
Horizon initiated and conducted the research in the public interest at its own cost.
Horizon has partnered with the School of Population Health in a number of surveys since September 2020 on New Zealanders’ attitudes to COVID-19 vaccines accurately measuring and projecting vaccine uptake.
Methodology
The online study conducted between 30 November and 6 December 2021. Respondents are from Horizon’s nationwide adult and Māori adult online research panels and a third party panel used for source diversity. The total sample size was 1,022 adults, 18 years of age and over.
The data was weighted on age, gender, level of education, employment status, region and ethnicity to be representative of the adult New Zealand population at the 2018 census.
The maximum margin of error is ±3.1% (at the 95% confidence level) overall.
For further comment please contact:
Professor Chris Bullen, Professor of Public Health at the University of Auckland’s School of Population Health, email c.bullen@auckland.ac.nz, telephone 021 425 267.
Graeme Colman, Principal, Horizon Research, email gcolman@horizonresearch.co.nz, telephone 021 848 576
For further information please contact:
Andrew Stevenson, Manager, Horizon Research, email Andrew.stevenson@horizonresearch.co.nz, telephone 021 464 307
HorizonPoll Online Survey system
and website developed by BEWEB
Copyright © 2010. HorizonPoll incorporating ShapeNZ - Listening to New Zealand


